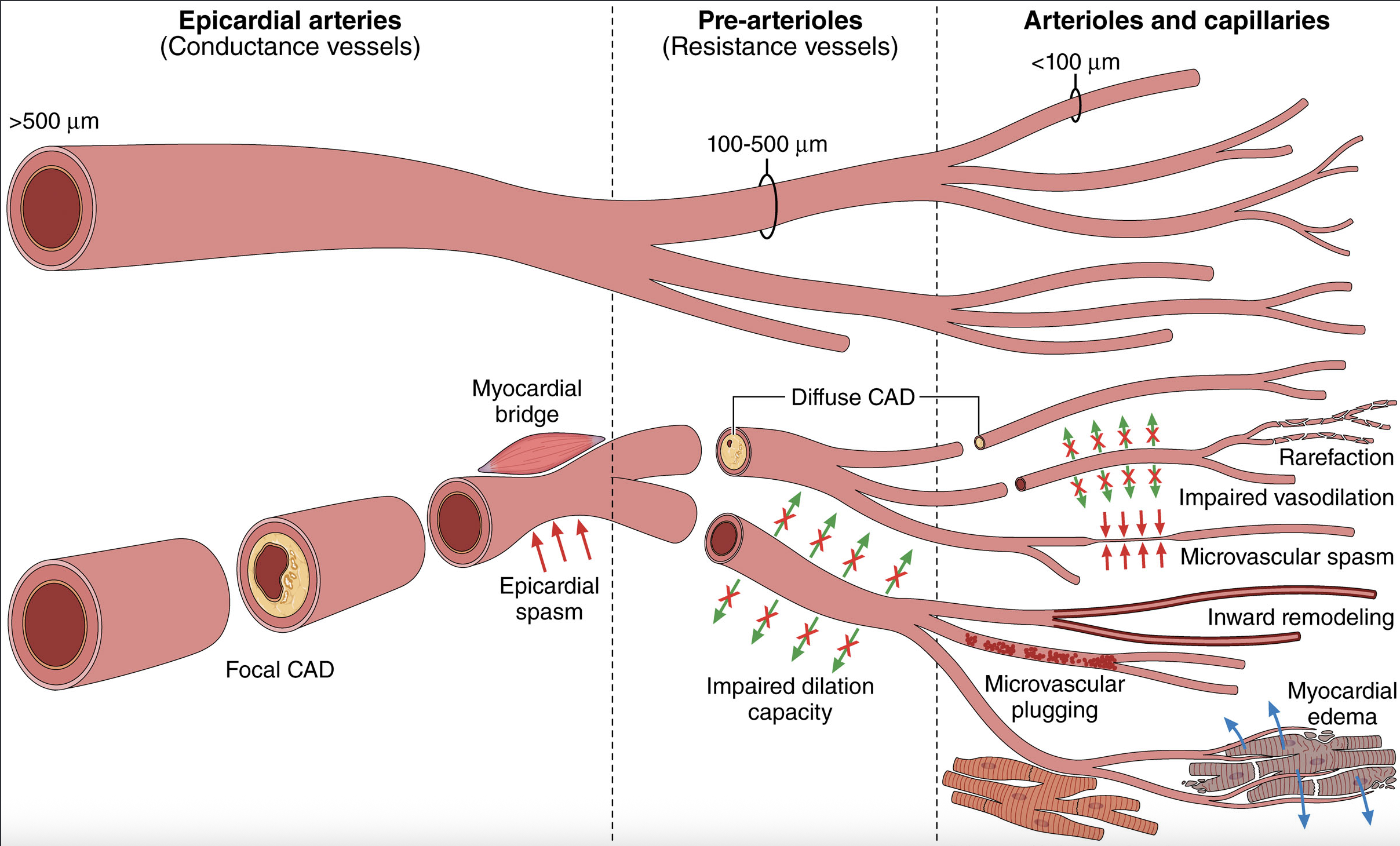
CMD affects the heart’s smallest blood vessels — pre-arterioles and intramyocardial arterioles — accounting for over 75% of coronary resistance. Despite being invisible to standard angiography, CMD contributes significantly to ischemic symptoms and long-term outcomes.
According to the review, nearly 50% of patients undergoing coronary angiography for angina do not have obstructive disease. Among these, CMD is frequently the cause of symptoms and adverse events.
Key diagnostic metrics:
- Coronary Flow Reserve (CFR): CFR < 2.0–2.5 suggests CMD.
- Index of Microcirculatory Resistance (IMR): IMR ≥ 25 indicates elevated microvascular resistance.
Acetylcholine testing reveals vasospasm or endothelial dysfunction. CMD is suspected when microvascular flow increases
CMD is also implicated in myocardial infarction with no obstructive coronary arteries (MINOCA), heart failure with preserved ejection fraction (HFpEF), Takotsubo syndrome, and persistent angina following percutaneous coronary intervention.
In HFpEF cohorts, 66% of patients had CMD. In STEMI, 50% showed microvascular obstruction despite revascularization.
Guidelines now recommend CMD assessment for INOCA, with the European Society of Cardiology (ESC) and American Heart Association (AHA) supporting CFR/IMR and acetylcholine testing.
The review calls for wider adoption of CMD testing, improved clinician training, and targeted therapies. Ongoing trials such as PRIZE and STRIVE aim to fill current therapeutic gaps.
Conclusion: CMD is now a recognized and measurable contributor to ischemic symptoms, and its systematic assessment is increasingly supported in clinical cardiology.
References
Smilowitz NR, Toleva O, Chieffo A, Perera D, Berry C. Coronary Microvascular Disease in Contemporary Clinical Practice. Circ Cardiovasc Interv. 2023;16:e012568. doi:10.1161/CIRCINTERVENTIONS.122.012568